Fluids contacting a boundary layer, in this case nasal tissue, impart a stress between the stationary tissue and the moving fluid (in this case air). Normal stress arises from a force vector perpendicular to a surface like pushing against a wall while shear stress arises from a force vector parallel to the surface. The impact of this stress interaction on the tissue by air can be measured in fluid dynamics. These results can give us an idea of the “tugging” forces involved on tissue in different parts of the nose. The trigeminal nerve branch extends into the nasal cavity and has been thought to possess both thermal and mechanical pressure sensors which provide feedback to the brain to help regulate autonomic breathing. You can override your breathing while awake but while sleeping autonomic breathing is in control. My sleep results section proves this is not theory but fact. With ENS there is simply too great of a loss of both mucosa tissue and nerve sensing capability. This loss raises the threshold for the proper activation of the nasal-pulmonary reflex. Not only is there reduced velocity and reduced shear stress, but less tissue to even interact with it. Subtle changes therefore can have an unexpectedly larger impact. Shear stress can be expressed in units of Pascal or “Pa” as seen below.
Shear Stress Results: Prior to any Surgeries 5L/minute (images 1-5) Shear Stress Results: After first Surgery 5L/minute (images 1-5)
Shear Stress Results: After first Surgery 5L/minute (images 1-5)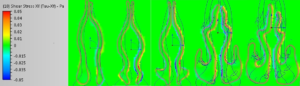 Shear Stress Results: After second Surgery 5L/minute (images 1-5)
Shear Stress Results: After second Surgery 5L/minute (images 1-5)
Continued (Images 6-9)
Shear Stress Results: Prior to any Surgeries 5L/minute (images 6-9) Shear Stress Results: After first Surgery 5L/minute (images 6-9)
Shear Stress Results: After first Surgery 5L/minute (images 6-9)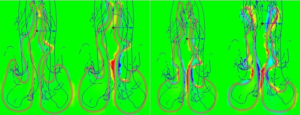 Shear Stress Results: After second Surgery 5L/minute (images 6-9)
Shear Stress Results: After second Surgery 5L/minute (images 6-9) 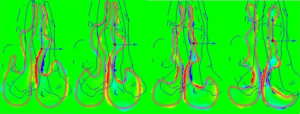
Key Findings:
These moves are (once again) not subtle, they are extreme in magnitude. As can be seen above, the sub-total turbinectomy has impacted the levels of shear stress even anterior to the main area of actual tissue loss. There is generally far less shear stress in the upper nose. If we remember again that the left side was “normal” we can see that the right side certainly exhibits a higher amount of shear stress as the model process has commanded that a fixed flow rate be pulled through a narrower right side model, HOWEVER, we can also see that overwhelmingly, previous areas of “normal” contact with the walls are now negligible or even non-existent post-surgery. By mid-cavity in image #6 there is almost nothing left to measure on the same scale setting of +/- 0.05 Pascals. The removal of inferior turbinate tissue has changed the localized amounts of the entire “system”. While many areas have decreased, some areas have increased. It is unknown by me but quite possible that perhaps some stresses may now be in areas that were not meant to handle such stresses.
The image results for shear stress are a little harder to interpret and give “easy” graphical results for but they yield some valuable clues. The biggest difference that catches my eye is that by 2011 (post 2 surgeries) there is far more shear stress posteriorly (images 6,7,8,9) than was the case originally. Much of this force is on the septum. Pre-surgical intervention, things were pretty diffuse by the ¾ model point (ignoring the obstructed right side turbinate). This is basically air coming straight in and slamming into the posterior which matches my symptom of feeling cold air hitting the back of my throat after the second surgery. Objectively I can certainly report large changes in the amount of forces and the distribution of those forces but I can’t offer too much else other than to present the data and allow others to draw their own informed conclusions.
Dr. Marc Oliver Scheithauer had this to say regarding shear stress and ENS in his study “Surgery of the Turbinates and Empty Nose Syndrome”:
“It is accepted that optimum pressure values within narrow limits in healthy people trigger both mucus production in the goblet-cells as well as the ciliary function in order to regulate mucociliary clearance on a cellular level. The precondition for this procedure is a correct balance of pressure values or shearing force on the nasal mucosa [238]. In the case of patients with ENS, these regulation mechanisms are disturbed by altered shearing forces; the pressure profile curves show a more rapid drop on the pressure gradient between the anterior and posterior nasal sections. The surgical reduction of the nasal cross-section in order to positively influence aerodynamics and to increase airway-resistance does not, however, alter the conditioning function of the nose, which is irreversibly damaged [220]. The reconstruction or transplantion of the missing respiratory mucosa is not possible at present. For this reason, patients profit only to a limited degree from so called “endonasal augmentation surgery”.
