I have learned a lot about nasal aerodynamics (against my will) and now I feel very confident in sharing all that I have learned about “repairing” Empty Nose Syndrome. I have seen a lot of CFD studies and even many CFD scans of individuals, but what can be learned about actually “fixing” them from looking at a single “result” ??? Answer: Not much!
To truly “fix” this condition it must be understood and that is only done through “characterization” or making iterations of changes to the models to gauge the effects of various “fixes” which is time consuming and expensive. This study accomplishes that task and in great detail. I learned some basic rules that apply to everyone not just me. They are actually quite easy to understand and follow but “proving” what they are requires some serious explaining so grab some coffee, get comfy and GET READY TO WORK!!!.
If you find this information valuable to you please consider donating to help support my work here. THANKS!
When I speak of “fixing” and “repairing”, I speak only in terms of “somewhat” restoring mechanical/physiological form. This does not replace missing nerves or restore functional missing mucosa tissue or cilia function, HOWEVER, addressing mechanical flow CAN and DOES help with most issues that torment ENS patients. It helped me with Dryness, sensation, nerve pain, suffocation, anxiety, muscle weakness, mental panic and sleep!
These symptoms are helped by:
- Restoring more normal pressure levels,
- Creating “smart” resistance (even and systemic, from front to back, not pinched at one point),
- Distributing forces more evenly and avoiding force concentrated on one area
- Increasing velocity in previous areas of dead flow by restoring some semblance of balance,
- Facilitating more actual air contact with the tissue.
This list alleviates a lot of problems created by what I feel are excessive, inhumane and just plain retarded nasal surgeries that leave patients orders of magnitude beyond normal human levels for critical parameters like pressure, velocity, shear stress and thermal warming capacity.
The last point before diving in head first is that these fixes rely on what is “surgically possible” by a small handful of highly skilled doctors and is also limited by the materials used. Dr. Steven Houser first blazed a path by fighting decades of conflicting studies and hardened opinions based on those studies. I was lucky to find Dr. Jayakar Nayak at Stanford who has really taken on the task of scientifically understanding and mechanically fixing this condition. Kudos go out to Stanford University as well for supporting him. Dr. Subinoy Das has taken on a large role. On the research front there are (and have been) many great researchers like Dr. Kai Zhao who just completed a study to help us. There are a handful of others around the world who can also help.
If you got this far and don’t know what we are fixing then refer to: This, this, this, this, this, and this.
Modification#1 was a key for me. If your Inferior heads were amputated, then large implants right up front in the cavity may help you. Dr. Nayak’s cotton test proved this for me and it was backed up by modeling results. The natural design was a large soft radius gap that transitions to a free hanging turbinate that evenly distributed air into the upper, middle and lower nose. The best we can do now is to have the lateral walls bulged out. This creates a very different distribution pattern than the original design but it’s all we have now. 

I ran about 30 different models early on exploring various cavity implant sizes and locations that I thought were “possible” and wasn’t able to get a normal distribution from any of them until this model above. Dr. Nayak pressed a bunch of wet cotton into this area and it felt good. I went outside a jogged a little and I was not out of breath! He then implanted this location heavily with Alloderm and he hit a home run. It took him (and his team) 4 HOURS of surgery to try to reverse what was snipped off with scissors in 15 minutes. He gently loosened up the dry sclerotic tissue off the bone which he said was “tight as a drum”. If it tore, the implants would not have been possible. Dr. Nayak is a ROCK STAR.
Modification#2 is leaving the anterior heads from above alone (I hope you have yours) and adding larger cavity implants that extend further back along the cavity. I was conservative here, larger would have been better. I modeled what I thought was possible. One major rule I learned is that if you have a “sharp” feature like a narrow valve or a big implant up front WITH an empty cavity behind it, then that creates turbulence after the feature into the empty cavity. (refer to 2011 left 3D CFD traces image in results section) Air needs to be narrowed down in the outer nares, compressed and evenly distributed at the heads AND guided in the cavity. These modeled implants provide some extra guidance.

Modification#3 is restoring my Septum back to normal. This is unfortunately impossible for me because my septum was hacked down to a 1.76 mm thin flap of skin with a small hole in it. I think they missed a spot! If you had a septoplasty AND turbinectomy together then that probably brought you here to my site. Many ENT doctors seem to feel that septoplasties are a harmless add on. I disagree and Dr. Marc Oliver Scheithauer said he is focusing on septoplasties as a likely cause of ENS. We will get to results next but here is: 1) the solid model I ran, 2) the actual CAD model measurements from my prior life before any surgeries and 3) a scope image of what some ENT doctors do to nasal septums.


RESULTS
Some people are visual and understand CFD color images with traces and some people like graphical chart results. Dr. Nayak’s eyes glazed over when I made him look at some CFD images but he loves graphs and hard numbers. I will present something for everyone. Skip through this section to find your own preferential way of understanding the results.I’ll start with pretty pictures since graphs bore or scare most people away. These results ALL use the same scale setting (Velocity 200cm.second) so changes can easily be seen and compared. Before I show the modifications let’s start with a complete history of all surgeries including my Implants!!! (yes finally)
RESULTS: Actual Surgical History (RIGHT SIDE) 3D CFD images with traces



RESULTS: Actual Surgical History (LEFT SIDE) 3D CFD images with traces
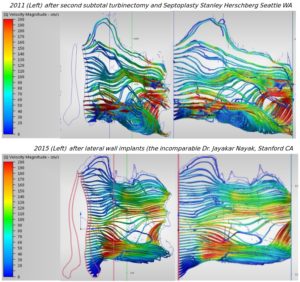

The difference between 2011 when I was suicidal and 2015 after Dr. Nayak’s implants are VERY striking to say the least. Look at both sides, 2011 to 2015 and the graphs to follow and you will see that he solved all of our primary goals I set out pretty well: (1) restoring more normal pressure levels, (2) creating “smart” resistance (even and systemic from front to back, not pinched at one point), (3) distributing forces more evenly and avoiding force concentrated on one area (4) increasing velocity in previous areas of dead flow by restoring some semblance of balance, (5) facilitating more actual air contact with the tissue. So who is cooler now? Dr. Nayak or some rock singer?
Unfortunately, you can also see that the Alloderm implants shrank quite a bit over 22 months as measured in 2016, BUT…. I am STILL WAY better off today as I type 2.5 years later. I can remember going to lunch in 2012 and having panic attacks so bad that I was laying in the booth at restaurants during lunch time. I was laying on the floor of my lab once or twice a day while trying to work. I didn’t sleep much and what little I got I was pounded while asleep. Any physical activity at all sent my heart racing, even walking up 5 steps going to work. So, THANK YOU to Dr. Nayak and to Stanford U. because I am so much better now.
RESULTS: Graphical Numerical Results (Right Side)
I started with the right side because it is an example of “classic” Empty Nose Syndrome. It is the larger side. The graphs below are a COMPLETE surgical history for Pressure readings. Why is proper pressure a big deal? because a higher negative pressure induces wider opening of distal bronchioles which is necessary for proper alveolar gas exchange in the lungs. Nasal resistance during expiration also helps maintain lung volume.
The “Color Key” for these graphs is: 2006 was life before any surgeries, 2007 after surgery 1, 2011 after surgery 2, 2015 after Implants and 2016 was 22 months after implants. I use this convention throughout so my easy way to remember is: Blue =before, Red =when is red ever good? Black = Death, Green = Good, and Purple = Present
I added 2 dashed blue reference lines and green target area boxes to show where “Normal” SHOULD be. (proof later)
 The right side was indeed obstructed but as you can see the first surgery alone put me from -38Pa all the way down to -2.94 Pa (close to zero huh?) That was a 92% drop and the second surgery (as if possible) put me at -1.5 Pa or near ZERO resistance for a 96% drop. Perhaps a Tracheostomy would get me to zero? Is there anything in-between for these guys? There was a LOT of space on that graph to land elsewhere. Do they have some kind of a “standard” scale for obstruction and an idea what each type of procedure actually does to dispense the required care? The answer is NO. They also seem to do everything BILATERALLY (both sides) whether it needs it or not. This shows me that some ENT doctors have no idea of the kind of subtlety and finesse that is required for good “human”results.
The right side was indeed obstructed but as you can see the first surgery alone put me from -38Pa all the way down to -2.94 Pa (close to zero huh?) That was a 92% drop and the second surgery (as if possible) put me at -1.5 Pa or near ZERO resistance for a 96% drop. Perhaps a Tracheostomy would get me to zero? Is there anything in-between for these guys? There was a LOT of space on that graph to land elsewhere. Do they have some kind of a “standard” scale for obstruction and an idea what each type of procedure actually does to dispense the required care? The answer is NO. They also seem to do everything BILATERALLY (both sides) whether it needs it or not. This shows me that some ENT doctors have no idea of the kind of subtlety and finesse that is required for good “human”results.
The green boxes above are for “NORMAL Human Pressure target levels”. How do I know what “Normal” is??? First, because my pre-surgery left side was normal and without issues. There was nothing wrong with it! Pressure there was -11Pa which calculates out to a resistance of 0.13 Pa/cm^3 (normal) Secondly because I also “modeled” a correctly performed SMR for my right side (here) (blue dashed line 1 for reference) which had a pressure of -22 Pa and a calculated actual “resistance” of 0.26 Pa/cm^3/second) which was NORMAL! (shown below)

“It has been reported in the literature that the mean total resistance in normal subjects ranges between 0.15 and 0.39 Pa/cm3/s (49), with a mean of 0.23 Pa/cm3/s. For this reason, a total nasal airway resistance of 0.3 Pa/cm3/s is accepted as the upper limit of normal (50). ”
Read More: http://www.atsjournals.org/doi/full/10.1513/pats.201005-034RN#.V8tsct9yv8g
So who is closer? doctors doing turbinectomies leaving people at 0.05 (which is below normal human specification) or my modeled SMR at 0.26 right near the 0.23 mean??? My modeled SMR was SPOT ON, so I win. (Thank You)
So let’s go ahead and create a “SPECIFICATION” since doctors don’t follow any and let’s call a “normal human target range” for pressure to be -10 to -20Pa. It is the job of ENT doctors to leave people somewhere inside a normal human target range, not to bore holes through their heads obliterating all resistance.

RESULTS: SURGICAL REPAIR MODIFICATIONS 3D CFD images with traces
Now let’s (finally) look at the “modifications” which I added to my present condition 2016 model to try to fix this mess for myself and others. I explored all of the ways I thought were surgically possible to improve flow back even closer to “normal”. While life is a LOT better, I am still missing a huge chunk of my life. I can limp through life and make it through work with far less overtly negative symptoms but I still can’t process air or handle much physical activity without being out of breath. If I worked in construction I would be disabled. This should help anyone searching for help for their own condition. It gives very clear visual answers for what each part of the nose does and what you need to reverse the damage done by aggressive nasal surgeries. I’ll present the images first, then discuss them and present the data as well.
Pay attention to the following: In the following images from left to right, observe how flow increases in the upper and middle nose and notice how flow (and force) is distributed more evenly and UNIFORMLY spread throughout the nose. The scale is the same 0-200cs/sec from above on all. Remember our objectives: (1) restoring more normal pressure levels, (2) creating “smart” resistance (even and systemic, from front to back, not pinched at one point), (3) distributing forces more evenly and avoiding force concentrated on one area (4) increasing velocity in previous areas of dead flow by restoring some semblance of balance, (5) facilitating more actual air contact with the tissue.
MODIFICATIONS: Measured Velocity (RIGHT SIDE)






MODIFICATIONS (LEFT SIDE)






RESULTS: MODIFICATIONS 2D CFD Images
The 3D model views above with traces show the actual path nicely and yield clues that 2D images don’t but some may prefer flat 2D images. This is where my velocity measurements come from since it is easier to measure lower, middle, upper nose by eye this way dividing into 1/3 sections.


RESULTS: Graphical Results from MODIFICATIONS (Pressure)
The “Color Key” for these graphs has an Olympics theme! Mod 1 (Anterior Heads Gap) = BRONZE Medal, Mod 2– (Reducing Anterior Heads gap AND Larger Cavity Implants) = SILVER medal, Mod 3, (fixing the Heads, Adding longer Cavity Implants AND bulking the Septum back to exactly where it was prior to ENT doctors) = GOLD Medal. It works! You’ll see! 🙂 I removed the two destructive surgeries (for clarity) and because they totally sucked and I added only the 2015 Implant surgery and where I settled to in 2016 so we can more easily gauge the benefits of these modifications.


RESULTS: Graphical Results from MODIFICATIONS (VELOCITY)
I think the 3D tracer images best show the changes in actual flow but if you don’t “groove” on those, here are the graphical chart results for velocity. The OBVIOUS thing here is this concept of the nose just being 3 pipes on top of each other but connected is how to view this. When you over open the largest lower pipe, it drops flow from the middle and upper ones. Literature says that most of the air we breathe travels in an arc through the middle of the nose. If you lost flow in the middle and you have nerves left there then guess what happens when you fill the bottom one back in??? and just how important is that septum after all??? Take a peak at the Upper and Middle nose for your answer!


Making sense of Results:
As you saw in the graphs above, Septoplasties totally fuck up the human nose. When I added a “normal” septum back into the model the anterior velocity profiles rocketed upwards for the upper and middle nose. I already mentioned they were a bad idea (here) so this is even more concrete proof for any remaining thick skulled doctors still in denial about ENS and the role they have in causing it.
I don’t think I can add too many more words to what I have shown here. I have been modeling for 4 years now and it’s hard for me to tell what others understand or don’t understand. I will just walk through some highlights and show what I see if that helps.
For the right side which was worse (more open), I see a MAJOR transformation as each “MOD” is added. The heads increased velocity and better distributed the air without obstructing as there are no bright red areas of saturation like 2011. It is increased but even. Then MOD2 implants show lower flow turning from blue to green. (going up and guided) I was totally blown away by the MOD3 septum and how that made almost the entire nose EVEN. The over saturated RED drill of 200cm/sec + air (actual measurement was over 300cm/sec) through the center of my nose from 2011 is gone. The turbulence from 2011 is gone. The dark blue (low flow) from the upper nose in 2011 GONE! 
Ditto for the left side but the issue here is that the septum is closer to the left side so the left is narrower. The valve is a little tighter and that creates some real turbulence in the cavity unless the implants are large enough. The pattern here at the heads area for both sides is NOT normal. It is the best we can do now without free hanging turbinates! To illustrate this point one only has to look below. Prior to any surgeries the air was pretty freaking even flowing AROUND the inferior turbinate and swirled upward mid cavity then down distributing the load nicely against the walls of the cavity. The first surgery alone completely fucked that up. I see a direct hole through, no distribution and serious turbulence with intense red flow all the way at the back of the nose. This is stupid shit folks! Turbinectomies are stupid shit. The second surgery only made it even worse.


The 2015 implants were great but the left came a little too far up into that super narrow area. I had Dr. Nayak do a very minor RF shrinking of that very front part and a tiny bit off of the left side septum because it can’t be moved. There is not much left of it. He knows the meaning of finesse! That pinch point was actually causing me some nerve pains that radiated from my nose into my left eye and on bad days, into my brain. If I slept too long (no saline spraying) it HURT from too much force for too many hours. The tissue was dried out from years of getting slammed and couldn’t take the velocity and force hitting it. This “new design” for implants needs to be well distributed and even. There are NO other doctors I have seen that have Dr. Nayak’s patience, caring or understanding. He listened and it worked. Anyone else would have called me crazy. Some have! Like Dr. Eric Pinczower.

LESSONS LEARNED, RULES for fixing and PREVENTING EMPTY NOSE SYNDROME:
SYMMETRY. I did a whole post regarding symmetry here. People from all over the world have been sending me CT scans asking me what I think. I tell them that I am not a doctor. I offer what mechanical sense I can and tell them to have it verified with a cotton test simulation to be sure it works. The number one issue that I see most have in common is a lack of symmetry, either prior to surgeries or after. I won’t post their CT scans but here is what I looked like in 2011.

Which side do you think more air goes through? If you have less sensation then you need to use all that you have. Every night that I sleep, I wear a prosthetic clip that I made that mostly blocks the right side and I jam a cone into the left side. I still take sleep data to back this up but this proves ENS exists. I have air, plenty of air on that right side, but I have little to no sensation. My O2 stability and heart rate stability is way better with the clip and cone. Without it I can’t sleep more than 2 hours. Doctors need to look at symmetry prior to surgeries. Many do EVERYTHING bilaterally (both sides) even when there is no need which horrifies me. Striving for normalcy and balance should be their goals for surgery.
VOLUME DISPLACEMENT:
The number one thing I learned about nasal aerodynamics is that it is ALL about volume displacement. Early on, I saw some people mention “deflecting” the air upwards with implants and similar statements. The answer I found is that implanting/making sharp features whether on the septum or elsewhere may indeed deflect it but it induces turbulence unless there are even features behind it and throughout. The nose is simply 3 pipes on top of each other. A large one, middle one and a small one. They are all tied together and volumetric displacement on the lower effects the other two. I modeled ENS “IT” (inferior Turbinate) because that is what I have. For those with missing middle turbinates that balance would also be destroyed just in a different manner.
EVEN GAPS:
I used the term “Smart Resistance”. This is my name for even systemic resistance from front to back. Even gaps throughout are necessary for balance. If I could glue a thin sheet of paper anywhere along your 6cm long path, you couldn’t breath. I think of that as “dumb resistance”. Some may have an empty cavity and a pinched valve or vise-versa. Even a well intentioned implant in the wrong location could be a problem.
Over Opening the Cavity:
The turbinates and cavity curve downward. When doctors go “straight in” with tools, many invariably take a straight cut which leaves a big chunk missing out of the center of the cavity. This large increase in volume causes a loss in negative pressure. You will notice the extreme differences in mid cavity pressure before and after surgeries. My septum SHOULD have been moved over to center rather than thinned down to nothing as pressure is uneven.

SPECIFICATIONS and FAILURE ANALYSIS:

Would you want to get on a plane that was made with no specifications? Probably not. So then why would you want a nasal surgery from a group of doctors who have ZERO specifications for a desired outcome? In my previous study I fully characterized the radial slit shape of the nasal cavity and found that: For every doubling of slit size in mm you lose roughly 50% in velocity, 85% of your negative pressure, and 72% of your shear force on the walls!!! Do doctors know the minimal conditions needed for a “normal” result or how close they leave you to either immediate or future latent failure? Doctors claim high rates of success (like around 3 million surgeries per year) but they don’t measure much hard data and claim that ENS is “rare”. If a car company sold 3 million cars a year but 0.05% of them had brake failures that killed people that is 1500 people! So how rare is “rare” ? 0.02% ? That is 600 people. There area 1200 victims on the YUKU Support group Forum and there are 1290 victims on the facebook support group. This issue is underreported. Maybe it is time that doctors come up with some actual numbers from their studies, identify the common threads of failure to determine safe operating procedures and set some guidelines going forward, THEN help repair people!
PREVENTION:
Of course the BEST “cure” for Empty Nose Syndrome is NOT CAUSING IT. Here is the modeled SMR I presented earlier as having “normal” pressure and resistance values on the pressure graphs. Doctors really need to do a proper informed consent for turbinectomies. They should admit that they have been studying this topic and arguing over inconclusive and conflicting studies for decades and that there is NO agreement on their value. (In engineering terms, they don’t have Jack Shit, yet they do this to people!)

The upper middle went from saturated red to yellow/green. The pinch point at the head of the inferior turbinate has been reduced and spread out more evenly. The whole middle/upper anterior went from yellow/red to a VERY even green.
Surgery impacts the nose in so many ways that the effects can cascade and yield non linear results. Surgery removes or damages nerves, changes flow patterns, destroys balance, reduces resistance, decreases negative pressure, decreases shear stress or puts it elsewhere and causes dryness which leads to loss of sensation of the coolness of evaporation during inspiration. It leaves less structure to deposit moisture during exhalation.
