Most nasal surgeries are indeed beneficial when done properly but there are certainly limits to their effectiveness and when those limits are crossed bad things can happen. When doctors over open a nose increasing the air gaps beyond this normal range there are MANY undesirable consequences which this study will fully document.
There is an “optimal” gap that allows air to pass while allowing some micro turbulence to occur which allows the air to properly contact the mucosa tissue. Air comes into the nose in a “laminar flow” then narrows down and turns “turbulent” at the nasal valve and heads of the inferior turbinates. It then is guided through the cavity contacting the turbinates and walls. Laminar flow, is smooth and orderly so only the outside edges of the air stream contact the walls just like a placid river. In an over opened nose the bulk of fluid gently flows right through the center with minimal contact with the rivers edge (outer walls).
A “Reynolds Number” (Re) is a term used to predict the threshold level where fluid flows turn from laminar to turbulent. The nose is DESIGNED to work with guided micro-turbulence and this is basically the crux of this entire site. There is NO MECHANICAL PURPOSE (or benefit) for over opening a nose beyond this critical width. A wider opening will have a far higher (Re). You can hear this for yourself. Breathe in slowly and listen….. Now breathe in a little harder. You will hear the transition point. For ENS victims, you can not breathe in (or out) hard or fast enough to even see this effect.You are beyond specification for this effect to occur with the normal amount of air that your lungs and diaphragm normally move. In short: We don’t need our nose turned into a second mouth.
Here is a quick layman’s guide to the concept of a Reynolds Number. (Skip to the paragraph on turbulent flow) It mentions that turbulent flow contains current eddies, that they mix and interact with each other and the walls and that they contain and transfer a lot of mechanical energy. Two factors that would raise (Re) are 1) increasing pipe diameter and 2) reducing roughness or (features). So what do “some” ENT doctors do? They flatten your septum and make it straight as an arrow, (removing features) and they cut turbinates to forge a gap big enough to pass peas through your nose. (larger pipe diameter and removing features) In that state, there will be no processing of inspired air, but let’s move forward.

In medicine there is however what is called the “Standard of Care” to protect patients and see they receive some kind of “STANDARD” of care: https://en.wikipedia.org/wiki/Standard_of_care#Medical_standard_of_care but, ironically the issue here of course is that there are no standards for nasal surgery in the first place.
In engineering and in the production of products, this is of course a recipe for disaster. Not having specifications or standards, with everyone following their own personal beliefs, doing things in whatever manner they see fit and to any degree they choose is surely a speedy recipe for complete failure. So why should this work in one branch of the medical field?
If you had a heart attack you would receive some very standardized care. There are no heart doctors who would cut out a heart valve trying to “increase flow” so why cut out and destroy a nasal valve which also has a purpose? I had conductive hearing loss in one ear. I saw a surgeon and he performed an operation called a “Stapedotomy”. This time I read up on the process and the doctor and everything went really well. They understand hearing. They KNOW what they are doing. They are all on the same page with what works yet with ENT doctors, many are still debating at conventions every year on how the nose even works.
Why should it be possible to receive completely different kinds of treatment for nasal obstruction depending on which doctor you see? It seems to me that most ENT doctors today do not know much about or consider aerodynamics but most realize that “being conservative” is the smart way to go. Unfortunately there are others who still seem to think that “more” is always better when it comes to surgery. Being conservative is an “unwritten rule” that should indeed be a written rule.
Compounding this problem of a lack of standards is that there are many different types of procedures for trying to reduce nasal turbinates by means of everything from electrical and RF (radio frequency) heating, to laser cutting, to “shaving” tissue and of course plain old fashioned cutting by use of a blade.
Cutting or “resection” procedures come with many different but perhaps similar sounding names like a septoplasty of the septum or a turbinoplasty or turbinectomy of the turbinates etc. These procedures may describe the amount cut or even the method used. A “SMR” can even be performed two completely different ways, one cutting along the bottom free edge, elevating mucosal flaps and removing some bone while the other penetrates the front only and removes material from within for the same “named” procedure.
Despite the fact that so many types of surgeries exist, like a mucosa tissue preserving SMR compared to a Total or a Sub-total Turbinectomy, (which is full thickness cutting and removal of 3 dimensional areas) there seems to be no guarantee that you wind up getting what you discussed and agreed to. Names of procedures seem to be used loosely and interchangeably. A lawyer friend stated to me that it appeared to him that “one man’s SMR was another man’s sub-total”.
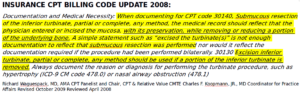
Despite this, surgical text books ARE indeed VERY clear on the delineations and the boundaries between these procedures (as are insurance CPT codes) so the results achieved are clearly planned and are far more a product of the individual surgeon’s “belief system” than by some kind of surgical accident. Here is the EXACT insurance CPT code guidance for an SMR compared to a sub-total or total turbinectomy. They are VERY specific because these procedures are totally different and studies favor SMRs as more effective and less risky than full thickness cutting, yet many doctors seem to be taking short cuts by doing Sub-totals while promising or referring to an SMR:
I have crippled people all over the world sending me CT scans. I see middle turbinectomies, inferior turbinectomies, I see people with BOTH! I see turbinectomies WITH additional septoplasties. I see holes in peoples sinuses. I see 3 and 4 procedures performed at the same time! I see burned turbinates, cut turbinates, Out-Fractured turbinates and even turbinates shaved off with micro-debriders which are basically Dremel tools with saw blades. Now to any person with common sense, it doesn’t pass even a basic sniff test that all of the above procedures applied in “wonton” fashion could ever provide normal human results. Clearly some of these ENT doctors are harming people.
Lastly, many ENS sufferers have also sadly received additional procedures that they never even discussed or agreed to. So though you may discuss and agree to some type of turbinate reduction procedure, you may unknowingly also receive an additional septoplasty. Conversely, you may also agree to have your septum “straightened” and wake up without turbinates as well. It is hard to say how often this happens. For me it was twice out of two or 100%. First I got a sub-total Turbinectomy after agreeing to an SMR described as a trim. Then, a second opinion doctor who assured me that “your issue is farther back” and would “trim a little more tissue farther back” gave me an overly aggressive septoplasty and another bilateral turbinate reduction from front to back after I agreed that he could “trim a little more turbinate tissue farther back”.
Of course the term “trimming a little tissue” was used by both so I learned the hard way that it is a “code term” to understate things and calm your very rational fears of surgery. This rather cavalier dispensing of surgeries of course goes against the required legal process of “informed consent” and I would like to see this issue stopped: https://en.wikipedia.org/wiki/Informed_consent#Elements_of_valid_informed_consent
The last way to get more surgery than you agreed to or want is simply by “Matter of degree”. Where does an SMR end and a subtotal begin? Should the inferior turbinate heads be reduced? if so by how much? Do you actually need a septoplasty AND turbinate reduction? The truth is that this branch of medicine is a woefully inexact “science” and has been the subject of much debate for 100 years. Each doctor is making individual and irreversible “guesses” during a 15 minute visit that will affect the rest of your life.
There have been a lot of turbinate reduction studies over the years and many conflict with each other. In engineering terms they have nothing. Conflicting studies mean there is no agreement. There are STILL some supporters of Total Turbinectomies to this day and of course they can all point to their favorite middle-east study that shows how great they are and “how people in the desert had theirs completely removed and they were fine” etc. while other studies point to the exact opposite conclusion.
Would these same doctors have their son or daughter receive a total turbinectomy? That is the question. It is great to be a fan of statistics and look at these intellectual and scientific studies and have some opinion on the matter but dispensing irreversible surgeries based solely on one side of these studies is another matter entirely. Uncomfortably, this topic is more akin to the dismal sciences of economics and politics where some have a staunch dogma about things which are in fact hard to accurately measure and prove.
In summary, while a lot of tremendous studies have been done by very smart people and their lessons are public knowledge, there is no guarantee that your doctor understands or even agrees with them. Unlike the ears or the heart, there is still some level of debate by some about exactly how the nose even works and how much it’s neural connections affect other areas of your health like sleep. It was extremely frustrating to me when I read studies that pointed out the same exact things that happened to me were known by some but not agreed on by all.
In engineering, when problems are unsolved, we put numbers on things to try to understand them. Through my work here, I hope to establish a baseline and some “standards” for what “aggressive” and “proper” actually are by examining the behavior of air through the nose, identifying key areas and determining safe limits which allow for some extra air flow without sacrificing the natural “design intent” of the nose or upsetting the natural distribution and interplay of each area.
